Corneal Disease
Blepharitis
 Blepharitis is a chronic inflammation – a long-term swelling – of the eyelids and eyelash follicles. It may be caused by seborrheic dermatitis, acne, bacterial infection, allergic reaction or poor eyelid hygiene. They eyes may become red, blurry or tear frequently. The eyelids crust, flake, scale or redden, and the smooth inside lining of the lids may become rough. In more serious cases, sores can form when the crusting skin is removed, the eyelashes may fall out, the eyelids can deform, the infection can spread to the cornea, and patients often suffer from excessive tearing. Blepharitis can also cause styes, chalazions and problems with the tear film.
Blepharitis is a chronic inflammation – a long-term swelling – of the eyelids and eyelash follicles. It may be caused by seborrheic dermatitis, acne, bacterial infection, allergic reaction or poor eyelid hygiene. They eyes may become red, blurry or tear frequently. The eyelids crust, flake, scale or redden, and the smooth inside lining of the lids may become rough. In more serious cases, sores can form when the crusting skin is removed, the eyelashes may fall out, the eyelids can deform, the infection can spread to the cornea, and patients often suffer from excessive tearing. Blepharitis can also cause styes, chalazions and problems with the tear film.
Treatment and preventative care for blepharitis involves thorough but gentle clea Save & Exit ning of the eyelids, face and scalp. Warm compresses can be applied to loosen crust and dandruff shampoo can help keep the eyelids clear. This may be combined with antibiotics if a bacterial infection is causing or contributing to the problems.
Cornea Transplantation for Corneal and External Eye Disease
The cornea is the clear covering on the front of the eye which bends, or refracts, light rays that focus on the retina in the back of the eye. A certain shape or curvature is required in order for light to focus exactly on the retina, rather than in front of it or behind it.
An improperly curved cornea may be corrected surgically or non-invasively to reduce or eliminate the need for eyeglasses or contact lenses. A thorough eye examination and consultation are necessary before a treatment decision can be made.
Corneal transplantation, or keratoplasty, is recommended when the cornea’s curvature is too steep or flat to be treated with other methods, or when extensive damage has occurred due to disease, infection or injury. Common problems that require transplantation are:
- Dry Eyes
- Blepharitis
- Recurrent Erosion
- Corneal Ulceration
- Herpes Simplex Keratopathy
- Pseudophakic Corneal Decompensation
- Keratoconus
- Corneal Dystrophies
- Pterygia
- External tumors
- Eye infections
- Traumatic injury
- Ocular surface diseases
- Chemical burn
Transplantation involves replacing the damaged cornea with a healthy one from a donor (usually through an eye bank). Keratoplasty is a low-risk procedure – it is the most common type of transplant surgery and has the highest success rate.
During the procedure, a circular incision is made in the cornea. A disc of tissue is removed and replaced with healthy tissue; these discs may be thin (lamellar keratoplasty) or as deep as the entire cornea (penetrating keratoplasty, the technique used in almost all corneal transplants). Local or general anesthesia may be used. The entire procedure lasts only 30-90 minutes.
DSAEK
DSAEK is the latest technique in corneal transplantation. Short for Descemet-stripping automated endothelial keratoplasty, DSAEK offers clear post-operative vision and short recovery time to patients in need of new corneas.
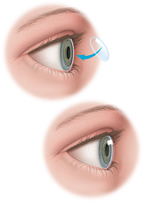
During the procedure, the surgeon makes a mark in the surface of the patient’s cornea with a trephine (an instrument used to cut circular sections of tissue). That mark serves two purposes: it helps the surgeon determine what size the transplant should be, and it outlines the area of the patient’s cornea that needs to be peeled away. Next, the surgeon scores the damaged section of the cornea and strips the membrane away from the eye. Then the donor cornea is folded into a “taco” shape and placed on the eye. A single stitch closes the incision.
Sometimes the new cornea unfolds on its own; other times, the surgeon unfolds it him/herself. When it is unfolded, a second stitch is made to close the wound and anchor the new cornea in place. The surgeon then injects an air bubble underneath the cornea, making sure it is centered on the eye, and dilates the pupil with eye drops.
Patients are sent to the recovery room for about one hour, after which they are examined at the slit lamp with the doctor. He or she gently presses on the cornea until most of the air bubble is released. Patients are then given antibiotics and steroid eye drops and will return the next day for a follow-up appointment.
Dry Eye
Dry eye occurs when the eyes aren’t sufficiently moisturized, leading to itching, redness and pain from dry spots on the surface of the eye. The eyes may become dry and irritated because the tear ducts don’t produce enough tears, or because the tears themselves have a chemical imbalance.
People usually begin experiencing dry eye symptoms as they age, but the condition can also result from certain medications, conditions or injuries. Dry eye is not only painful, it can also damage the eye’s tissues and impair vision. Fortunately, many treatment options are available.
Non-surgical treatments for dry eye include blinking exercises, increasing humidity at home or work, and use of artificial tears or moisturizing ointment. If these methods fail, small punctal plugs may be inserted in the corners of the eyes to limit tear drainage, or the drainage tubes in the eyes may be surgically closed. Eyelid surgery is also a solution if an eyelid condition is causing your dry eyes.
Excess Tearing/Watery Eyes
Although tears are necessary to lubricate the eyes and wash away foreign bodies and other particles, some people produce too many tears or cannot drain them properly, leading to excess tearing or watery eyes.
Tearing of the eyes can be caused by several different factors, including:
- Allergies
- Blepharitis
- Blocked tear duct
- Conjunctivitis
- Dry eyes
- Environmental irritants
- Foreign bodies
- Infection
- Irritation
- Trauma
Treatment for watery eyes depends on the underlying cause of the condition, but can often be treated at home. Artificial tears or anti-histamines may be recommended to treat dry eyes or allergies, while other causes may require antibiotics or even surgery to relieve symptoms.
Fuch’s Dystrophy
 Fuchs’ dystrophy is an inherited eye disease that causes the cells in the last layer of the cornea to deteriorate, leading to distorted vision and corneal swelling. The exact cause of Fuchs’ dystrophy is unknown, but is believed to be a combination of hereditary, hormonal and inflammatory factors. This condition affects both eyes and is more common in women than in men.
Fuchs’ dystrophy is an inherited eye disease that causes the cells in the last layer of the cornea to deteriorate, leading to distorted vision and corneal swelling. The exact cause of Fuchs’ dystrophy is unknown, but is believed to be a combination of hereditary, hormonal and inflammatory factors. This condition affects both eyes and is more common in women than in men.
The cornea is made up of five different layers, each of which has a specific function that controls vision.
The endothelium is the back layer of the cornea, which removes excess fluid from the stroma, the largest part of the cornea made up of water and collagen. Excess fluid can cause the stroma to swell and vision to become distorted.
When these cells deteriorate more rapidly than normal, fluid will continue to build up and vision will worsen. Once cells are lost, they do not grow back, so this condition will continue to progress with time.
Symptoms
Although this condition is inherited, symptoms do not usually appear until the patient is over the age of 50. Patients with Fuchs’ dystrophy may experience blurred vision as the first sign of this condition. Blurred vision occurs as a result of fluid accumulating in the cornea while you sleep. As this fluid evaporates throughout the day, vision will improve. Other symptoms of Fuchs’ dystrophy may include:
- Sensitivity to bright lights
- Halos around lights
- Poor night vision
- Sharp pains in the eyes
- Sandy, gritty sensation in the eyes
- Fluctuating vision
Treatment
While there is no cure for Fuchs’ dystrophy, there are several treatment options available to help relieve the symptoms of this condition and to prevent permanent damage. In its early stages, Fuchs’ dystrophy can often be treated with a salt solution to remove fluid from the eye and reduce swelling. Patients can also relieve excess fluid in the cornea by holding a hair dryer at arm’s length and blowing air towards the face. These methods are often successful in temporarily improving vision during the early stages of Fuchs’ dystrophy.
In more advanced stages, Fuchs’ dystrophy may begin to interfere with daily activities and prevent patients from functioning normally. In this stage, patients may require a corneal transplant to replace the cornea with full, thick layers that allows them to see clearly.
Keratoconus
 Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The cornea is the clear, central part of the surface of the eye. In patients with keratoconus, the cone-shaped cornea deflects light and causes distorted vision.
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The cornea is the clear, central part of the surface of the eye. In patients with keratoconus, the cone-shaped cornea deflects light and causes distorted vision.
Although many theories have been proposed, there is no definite known cause of keratoconus. Possible causes include genetics, a collagen deficiency, overexposure to ultraviolet (UV) rays from the sun, or excessive eye-rubbing.
Sign and Symptoms of Keratoconus
Keratoconus often begins to develop in the teen years to the early 20s, although it can develop at any age. Changes in the shape of the cornea occur gradually, usually over several years. In most patients with keratoconus, both eyes eventually become affected.
Keratoconus can be difficult to detect because it usually develops very slowly. Signs of keratoconus may include:
- Distorted and blurred vision
- Myopia (nearsightedness)
- Astigmatism
- Double vision
- Headaches due to eye strain
- Glare
- Light sensitivity
Your doctor will measure the curvature of your cornea to determine whether these symptoms are a result of keratoconus.
Treatment
In the early stages of keratoconus, glasses or soft contact lenses may help to correct the nearsightedness and astigmatism associated with the disease. As the condition progresses and the cornea becomes increasingly thin, more advanced treatment is required.
- Rigid Gas-Permeable Contact Lenses – If eyeglasses or regular soft contact lenses cannot control keratoconus, rigid gas-permeable (RGP) contact lenses are usually the preferred treatment. The rigid lens covers the cornea, replacing the cornea’s irregular shape with a smooth, uniform refracting surface, improving vision.Rigid contact lenses can be less comfortable to wear than soft lenses. Further, fitting contact lenses on a cornea with keratoconus can be challenging and time-consuming. If you are using RGP contact lenses, you will need to visit your doctor frequently to fine-tune the fit and prescription of the lenses, especially if your keratoconus continues to progress.
- Corneal Transplant Surgery – Surgery is needed for patients with advanced keratoconus, where other therapies no longer provide clear vision. This usually occurs in 15-20% of cases. In corneal transplant surgery, most of the cornea is removed and then replaced with a new donor cornea. The results of the procedure have a success rate of over 97%.
Pterygium
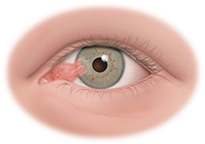 Pterygium is a benign growth of the conjunctiva (lining of the white part of the eye) that grows into the cornea, which covers the iris (colored part of the eye). It can eventually lead to impaired vision.
Pterygium is a benign growth of the conjunctiva (lining of the white part of the eye) that grows into the cornea, which covers the iris (colored part of the eye). It can eventually lead to impaired vision.
Patients with pterygium often first notice the condition because of the appearance of a lesion on their eye or because of dry, itchy irritation. Other symptoms include dryness, redness, irritation, inflammation, and tearing. In more severe cases, the pterygium grows over the pupil and limits vision.
The most common pterygium treatment is eye drops (artificial tears) and use of sunglasses. In more severe cases when vision is impaired, surgery may be recommended.


